Diarrhea in Children: Helpful Facts For Parents
Written by:
Joy Kimberly N. Militante MD, FPPS, DPSPGHAN
Pediatric Gastroenterologist

When your child is suddenly passing loose, watery, more frequent stools, he is having diarrhea. Diarrhea is one of the leading causes of Pediatric ER consultations and hospital admissions. Here are some of the common questions that you may have about diarrhea, including helpful tips on how to manage it and when you should call your doctor.
What causes diarrhea?
Diarrhea is most commonly caused by viruses like Rotavirus, Norovirus, or Adenovirus. It can also be caused by bacteria (Salmonella, Shigella), parasite (Entamoeba histolytica), changes in the diet (drinking too much fruit juice), and use of certain medications like antibiotics.[1,2]
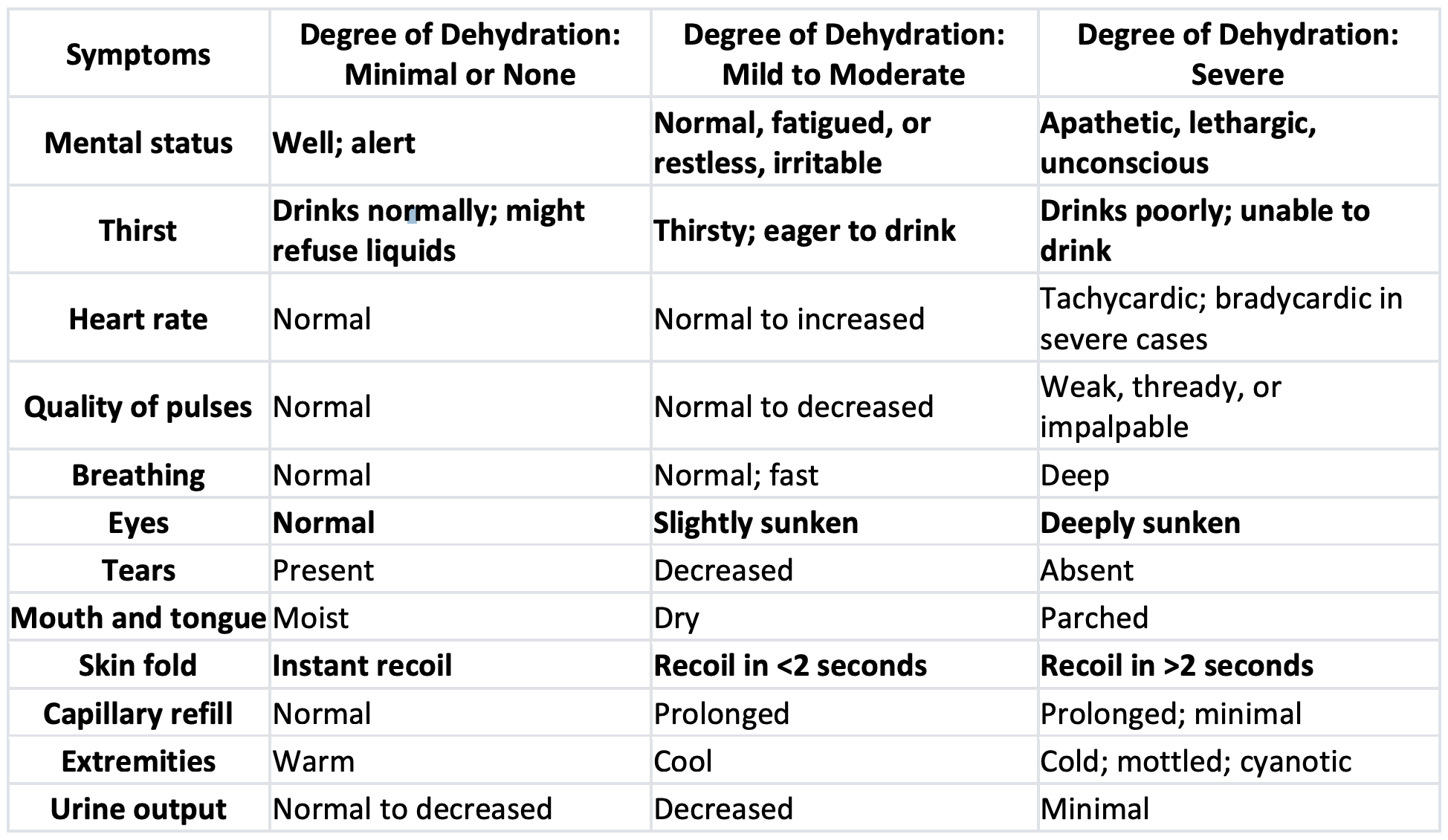
How do I know if my child is dehydrated?
Dehydration is a spectrum from minimal to none, mild to moderate, and severe. This can be assessed by 1) looking at a child’s mental status, 2) checking for sunken eyes, 3) offering a child drink and seeing if he drinks it eagerly or poorly, and 4) pinching the skin of the abdomen to see if it goes back quickly or slowly. The table below highlights the above 4 symptoms with their corresponding degree of dehydration. There are many other symptoms of dehydration, but it might be helpful to memorize the above 4 symptoms to help us rapidly assess a child.[3,4]
Table 1. Signs and Symptoms of Dehydration
What should I do if my child has diarrhea?
The primary goal of treating any form of diarrhea is to prevent dehydration. Dehydration is best managed by offering our child ORS 75, a commercially available low-osmolality drink containing 75 meq of sodium, 64 meq of chloride, 20 meq of potassium and 75 mmol of glucose per liter.
ORS 75 is designed to contain the appropriate amount of glucose and electrolytes to maximize fluid absorption in the small intestine.
ORS 75 is given to replace each diarrheal stool or vomiting episode. For infants and children <10 kg body weight: 50 – 10 ml ORS is given while for >10 kg body weight: 100 – 200 ml ORS is given in slow sips for every diarrheal stool or vomiting episode. Children with vomiting may benefit from small volumes of ORS given initially by a dropper, teaspoon, or syringe beginning with as little as 5 ml at a time. The volume is increased as tolerated.[1]
What is the mechanism behind ORS 75?
ORS75 is designed to contain the appropriate amount of glucose, electrolytes and osmolarity to maximize fluid absorption in the small intestine.[5] Plain water fails to replace the electrolytes lost in diarrhea or vomiting.
Can I give my child sports drinks to prevent dehydration?
Sports drinks, soda beverages, fruit juices, tea and other home fluids are not suitable for rehydration or maintenance therapy because they have inappropriately high glucose concentration and osmolarities and low sodium concentrations.[1] The composition of these drinks is not suitable to replace the gastrointestinal losses of diarrhea.
Should I give anti-diarrheal agents like Loperamide?
Over-the-counter anti-diarrheal agents like Loperamide are not recommended and can even be harmful for the child. These agents may have adverse effects like drowsiness, nausea, and ileus – the medical term for a temporary lack of normal muscle contractions of the intestine.[2]
Should my child fast (or NOT EAT) when he is having diarrhea?
Fasting is not recommended for children with diarrhea. Breastfed infants should continue nursing throughout their illness. After rehydration is complete in about 4 hours’ time, an age-appropriate normal diet should be offered every 3 – 4 hours. Diluted formula milk does not offer any
benefit.[1]
When should I seek consultation for diarrhea?
Consult with your doctor right away if your child shows any signs and symptoms of dehydration (see Table 1). Also call your pediatrician if you note any of these warning signs[2]:
- Diarrhea with fever that lasts longer than 24 – 48 hours
- Bloody stools
- Vomiting that lasts longer than 12 – 24 hours.
- Vomit that looks green, blood-tinged or like coffee-grounds
- Abdomen that looks swollen or distended
- Child will not eat or drink
- Severe abdominal pain
- Any unusualities like rash or jaundice (yellow color of skin and eyes)
The aforementioned symptoms will warrant urgent consultation, but you may also consult with your doctor if the diarrhea lasts more than 24 – 48 hours. Your doctor will determine the cause of diarrhea and give the corresponding treatment, in addition to rehydration with ORS75.
How can I prevent my child from getting diarrhea?
1. Proper handwashing is one of the key things to prevent diarrhea since diarrheal agents can be spread through the hands. This requires the use of hand soap and enough water to rinse the hands thoroughly. All family members should wash their hands thoroughly during these times: 1) after defecation, 2) after cleaning a child who has defecated, 3) after disposing a child’s stool, 4) before preparing food, and 5) before eating.[2,4]
2. Vaccination – you can help protect your infant from rotavirus, the most common cause of viral diarrhea in children. Measles vaccination can also reduce the incidence and severity of diarrheal diseases. These vaccines will be given by your pediatrician or local health provider at the recommended age of the child.[4]
3. Avoid medicines, such as antibiotics, if they are not needed.[1]
4. Emphasize food safety. Food can be contaminated by diarrheal agents at all stages of production and preparation, so practice proper food hygiene as follows[4]:
- Do not eat raw food, except undamaged fruits and vegetables that are peeled and eaten immediately
- Cook food until it is hot throughout
- Wash and thoroughly dry all cooking and serving utensils after use.
- Keep cooked food and clean utensils separately from uncooked food and potentially contaminated utensils, and
- Protect food from flies by means of fly screens.
5. Avoid giving sugar sweetened beverages (SSB) like soft drinks/soda, fruit drinks, fruit-flavored drinks, sports, and energy drinks. These drinks do not have health benefits and may cause loose watery stools in children. Water is the ideal beverage for children at all meals and during the day. Whole fruit should be encouraged over fruit juice.[6]
I hope this article has enlightened you and armed you with the basic knowledge on what to do in case your child has diarrhea.
References: